Oral infections refer to infections that occur in the mouth and its associated structures. They can range from mild, localized infections to more severe conditions that affect the entire oral cavity.
The mouth is a complex environment that houses various bacteria, viruses, and fungi, both harmful and beneficial. When the balance of microorganisms is disrupted or when pathogens (disease-causing agents) gain the upper hand, oral infections can occur.
- Dental Abscess: This is a localized infection that can occur in the gums, around the root of a tooth, or in the jawbone. It is usually accompanied by swelling, pain, and sometimes fever.
A dental abscess is a painful and potentially serious dental condition characterized by a localized collection of pus caused by a bacterial infection. The infection typically starts at the root of a tooth or in the gum tissue near the root and can spread to surrounding areas if left untreated. There are three main types of dental abscesses:
- Periapical Abscess: This type of dental abscess occurs at the tip (apex) of a tooth’s root and is usually a result of untreated dental decay or a dental injury that allows bacteria to enter the pulp chamber.
- Periodontal Abscess: This type of abscess originates in the gum tissue (periodontal ligament) and is often caused by gum disease (periodontitis) or an infection that spreads from the gum pocket to the surrounding tissues.
- Gingival Abscess: A gingival abscess is limited to the gum tissue and does not involve the tooth root or periodontal ligament. It can result from foreign objects, such as food particles, becoming trapped in the gum, leading to an infection.
Symptoms of a dental abscess may include:
- Severe, throbbing toothache
- Swelling and redness of the gums or face
- Tender or swollen lymph nodes in the neck
- Difficulty swallowing or opening the mouth
- Fever
- Foul taste or odor in the mouth
- Pus drainage from the affected area
If you suspect you have a dental abscess or experience any of these symptoms, it’s crucial to seek immediate dental care. Dental abscesses do not resolve on their own and require professional treatment to eliminate the infection and prevent complications.
Treatment for a dental abscess typically involves:
- Drainage: The dentist may make a small incision in the abscess to allow pus drainage, relieving pressure and pain.
- Root Canal Therapy: For periapical abscesses, a root canal procedure may be performed to remove the infected pulp from the tooth, clean the canals, and seal them to prevent further infection.
- Periodontal Treatment: For periodontal abscesses, deep cleaning procedures, such as scaling and root planing, may be necessary to remove plaque and bacteria from the gum pockets.
- Antibiotics: In some cases, the dentist may prescribe antibiotics to help control the infection and prevent it from spreading.
- Tooth Extraction: If the tooth is severely damaged or cannot be saved, it may need to be extracted to eliminate the infection.
Prevention is essential in avoiding dental abscesses. Practicing good oral hygiene, regular dental check-ups, and promptly addressing dental issues can help prevent dental abscesses from developing.
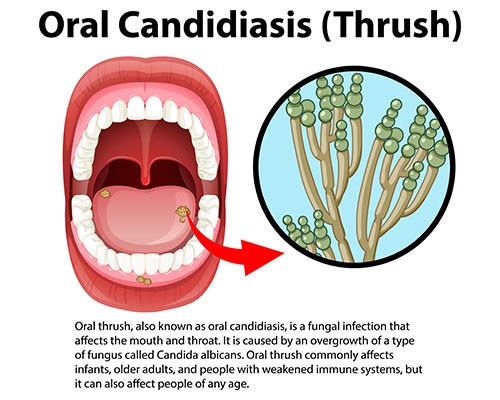
- Oral Thrush (Candidiasis): It is a fungal infection caused by Candida yeast. It appears as white patches on the tongue, inner cheeks, and palate. It can affect people with weakened immune systems, those on antibiotics, or individuals with certain medical conditions.Oral thrush, also known as oral candidiasis, is a fungal infection caused by an overgrowth of Candida yeast in the mouth and throat. Candida is a type of fungus that is normally present in small amounts in the oral cavity and gastrointestinal tract. However, certain factors can lead to an overgrowth of Candida, resulting in the development of oral thrush.Causes of Oral Thrush:
- Weakened Immune System: A weakened immune system due to illnesses like HIV/AIDS, diabetes, or certain medications can make a person more susceptible to oral thrush.
- Antibiotic Use: Antibiotics can disrupt the natural balance of microorganisms in the mouth, allowing Candida to overgrow.
- Corticosteroid Use: The use of inhaled or topical corticosteroids can increase the risk of oral thrush, especially in individuals with asthma or chronic respiratory conditions.
- Dentures: Ill-fitting or unclean dentures can create an environment favorable for Candida overgrowth.
- Dry Mouth: Reduced saliva flow can lead to dry mouth, which can increase the risk of oral thrush.
- Smoking: Smoking can weaken the immune system and create an environment conducive to fungal growth.
Symptoms of Oral Thrush: The symptoms of oral thrush can vary but may include:
- Creamy white lesions on the tongue, inner cheeks, gums, and the back of the throat. These lesions may resemble cottage cheese.
- Redness or soreness in the affected areas.
- Difficulty swallowing or a feeling of food getting stuck in the throat.
- Loss of taste or altered taste sensation.
- Dry, cracked corners of the mouth (angular cheilitis).
Treatment of Oral Thrush: Treatment for oral thrush typically involves antifungal medications, which can be prescribed as mouthwashes, lozenges, or oral gels. In more severe or persistent cases, oral antifungal medications may be prescribed.
Prevention of Oral Thrush: To prevent oral thrush, consider the following measures:
- Maintain good oral hygiene, including brushing your teeth twice a day and flossing daily.
- Clean dentures thoroughly and remove them at night to allow the gums to breathe.
- Limit the use of antibiotics and corticosteroids when possible and as directed by a healthcare professional.
- Quit smoking or avoid exposure to secondhand smoke.
- Manage underlying health conditions that may weaken the immune system.
If you suspect you have oral thrush, it’s essential to seek evaluation and treatment from a healthcare professional or dentist. Prompt treatment can help alleviate symptoms and prevent the infection from spreading or recurring.
Herpes Simplex Virus (Cold Sores): Cold sores are small, painful blisters that can appear on or around the lips, caused by the herpes simplex virus (HSV-1). They are contagious and can recur periodically.Herpes simplex virus (HSV) is a common viral infection that causes cold sores, also known as oral herpes or fever blisters. There are two types of HSV: HSV-1 and HSV-2. HSV-1 is the primary cause of oral herpes, while HSV-2 is typically associated with genital herpes. However, both types can cause oral or genital infections.Causes of Cold Sores: Cold sores are primarily caused by the herpes simplex virus type 1 (HSV-1). The virus is highly contagious and can be transmitted through direct contact with an active cold sore or by sharing items like utensils, towels, or lip balm with an infected person.Symptoms of Cold Sores: Cold sores typically go through several stages, and symptoms may include:
- Tingling and Itching: Before a cold sore appears, you may experience tingling, itching, or burning sensations in the affected area.
- Blisters: Small, fluid-filled blisters appear on or around the lips, mouth, or nose.
- Rupture and Oozing: The blisters may burst, releasing clear fluid and forming painful, open sores.
- Crusting: The sores eventually dry out and form a crust, which may last for several days.
- Healing: The crust falls off, and the cold sore gradually heals without scarring.
During an active cold sore outbreak, the virus can also be spread to other parts of the body, such as the eyes (herpetic keratitis) or to other individuals through direct contact.
Treatment of Cold Sores: There is no cure for the herpes simplex virus, but there are treatments available to alleviate symptoms and promote faster healing of cold sores:
- Antiviral Medications: Prescription antiviral medications, such as acyclovir, valacyclovir, or famciclovir, can help reduce the severity and duration of cold sore outbreaks when taken early during the onset of symptoms.
- Over-the-Counter Creams: Topical creams containing docosanol or lidocaine may help relieve pain and itching.
- Pain Relief: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help reduce pain and discomfort.
Prevention of Cold Sores: To reduce the risk of cold sore outbreaks and transmission, consider the following preventive measures:
- Avoid close contact with individuals experiencing a cold sore outbreak.
- Wash hands frequently, especially after touching cold sores.
- Refrain from sharing items that come into contact with the mouth, such as utensils, lip balm, or towels.
- Use sunscreen on the lips and face to protect against sun-induced triggers.
- Manage stress levels, as stress can sometimes trigger cold sore outbreaks.
If you experience frequent or severe cold sore outbreaks, consult with a healthcare professional or dermatologist. They can provide appropriate treatment options and help you manage the condition effectively.
- Hand, Foot, and Mouth Disease (HFMD): Although more common in children, HFMD can also affect adults. It is caused by various enteroviruses and presents with sores in the mouth and a rash on the hands and feet.Hand, Foot, and Mouth Disease (HFMD) is a common viral infection that primarily affects infants and young children. It is caused by various enteroviruses, most commonly the Coxsackievirus A16 and Enterovirus 71. HFMD is characterized by the development of small, painful sores or blisters in the mouth, on the hands, and on the feet. It is highly contagious and spreads through direct contact with an infected person’s respiratory secretions, saliva, feces, or fluid from the blisters.Symptoms of Hand, Foot, and Mouth Disease:
- Fever: HFMD usually begins with a fever, often ranging from 101°F to 103°F (38.3°C to 39.4°C).
- Sore Throat: Children with HFMD may have a sore throat or discomfort when swallowing.
- Mouth Sores: Painful red sores or ulcers may develop in the mouth, including on the tongue, gums, and inside the cheeks. These sores can make eating and drinking difficult.
- Skin Rash: A non-itchy rash with small, red spots or blisters may appear on the palms of the hands, soles of the feet, and sometimes on the buttocks.
- Irritability: Infants and young children may become irritable or fussy due to the discomfort caused by the mouth sores and rash.
- Lack of Appetite: Children may refuse to eat or drink due to the painful mouth sores.
HFMD is usually a mild illness, and symptoms typically resolve within a week to ten days. In most cases, the infection does not require specific medical treatment, and supportive care is usually sufficient. However, in some instances, especially when caused by Enterovirus 71, HFMD can lead to more severe complications, such as viral meningitis or encephalitis.
Prevention of Hand, Foot, and Mouth Disease:
- Hand Hygiene: Frequent handwashing with soap and water is essential to prevent the spread of the virus.
- Avoid Close Contact: Try to avoid close contact with individuals who have HFMD, especially if they have visible symptoms.
- Disinfect Surfaces: Regularly disinfect surfaces and objects that are frequently touched, such as toys, doorknobs, and light switches.
- Isolate Sick Individuals: Keep children with HFMD at home until they are no longer contagious to prevent the spread of the virus in childcare settings or schools.
If you suspect that your child has HFMD or if you or your child experience symptoms consistent with the disease, consult a healthcare professional for proper evaluation and management. While most cases of HFMD are mild and resolve on their own, seeking medical advice can help ensure appropriate care and prevent complications.
Oral HPV Infections: Human papillomavirus (HPV) can infect the mouth and throat, leading to the development of oral warts or, in some cases, an increased risk of certain oral cancers.
Oral HPV (human papillomavirus) infections are viral infections that affect the mouth and throat. HPV is a group of viruses, and there are more than 100 different types. While many HPV types cause no symptoms and go away on their own, some strains can lead to health problems, including oral infections.
Here are some key points about oral HPV infections:
- Transmission: Oral HPV infections are usually transmitted through intimate contact with the oral, genital, or anal areas of an infected person. This can occur through oral sex, kissing, or other forms of close contact.
- Symptoms: Most oral HPV infections do not cause noticeable symptoms, and the infection often goes away on its own without treatment. In some cases, the virus can cause lesions, warts, or other abnormalities in the mouth or throat. Persistent infections with high-risk HPV strains can increase the risk of certain cancers, including oral cancer.
- Risk Factors: Certain factors may increase the risk of acquiring oral HPV infections or developing complications from the infection. These risk factors include having multiple sexual partners, engaging in oral sex, smoking or tobacco use, and having a weakened immune system.
- Link to Cancer: Persistent infections with high-risk HPV strains, such as HPV-16 and HPV-18, can lead to the development of oral cancer. Oral cancers associated with HPV are most commonly found in the back of the throat, including the base of the tongue and tonsils. Regular dental check-ups can help detect any suspicious lesions or growths in the mouth.
- Prevention: Vaccination is the most effective method for preventing HPV infections, including those that can lead to oral cancers. The HPV vaccine is recommended for both males and females before they become sexually active, typically during adolescence. It’s important to get vaccinated before potential exposure to the virus.
- Screening: There is no routine test specifically for oral HPV infection. However, dentists and doctors can check for oral abnormalities during routine examinations. If suspicious lesions are found, a biopsy may be performed to determine if they are cancerous.
- Protection: Consistent and proper use of condoms or dental dams during oral sex can reduce the risk of transmission of HPV and other sexually transmitted infections.
Remember, most oral HPV infections do not cause any symptoms and go away on their own. However, it’s essential to maintain good oral hygiene and visit your dentist regularly for check-ups. If you notice any unusual changes in your mouth or throat, such as persistent sores, growths, or pain, consult a healthcare professional promptly. Early detection and treatment can significantly improve outcomes if oral cancer is suspected.
- 8. Canker Sores (Aphthous Ulcers): These are painful, round sores that can develop on the soft tissues of the mouth, including the inner cheeks, gums, tongue, and throat.Canker sores, also known as aphthous ulcers, are painful, non-contagious sores that can develop inside the mouth. They are a common oral health issue and can be quite bothersome, but they are not related to the herpes virus or cold sores, which occur on the lips or around the mouth. Canker sores can occur at any age but are more commonly seen in teenagers and young adults.Here are some key characteristics of canker sores:
- Location: Canker sores typically form on the soft tissues inside the mouth, such as the inner cheeks, lips, tongue, the floor of the mouth, and the back of the throat. They do not appear on the outer surface of the lips.
- Appearance: Canker sores are usually round or oval with a white or yellowish center and a red border. They can vary in size, from a few millimeters to more than a centimeter in diameter.
- Pain: Canker sores can be painful, especially when they are irritated by eating, drinking, or talking. The pain may be more pronounced during the first few days after the sore develops.
- Causes: The exact cause of canker sores is not well understood, but they are thought to be triggered by various factors, including minor injuries to the mouth (such as accidental bites), stress, hormonal changes, certain foods, and allergies. They may also be associated with some medical conditions, such as inflammatory bowel disease or celiac disease.
- Healing Time: Canker sores often heal on their own within one to two weeks without scarring. However, large or particularly painful sores may take longer to heal.
- Treatment: In most cases, treatment for canker sores focuses on managing the pain and promoting healing. Over-the-counter topical ointments or gels containing ingredients like benzocaine or hydrogen peroxide can help numb the area and provide relief. Additionally, avoiding spicy, acidic, and rough-textured foods can prevent further irritation.
- Recurrent Canker Sores: Some individuals may experience recurrent canker sores, where new sores appear before previous ones have fully healed. If you frequently suffer from canker sores or have particularly large or long-lasting sores, it’s a good idea to consult with a dentist or healthcare professional to rule out any underlying medical conditions.
While canker sores are generally harmless and resolve on their own, it’s essential to differentiate them from other oral lesions, such as cold sores, which are caused by the herpes simplex virus and require different management. If you are unsure about the nature of the sore or experience persistent oral health issues, seeking professional advice can help in getting an accurate diagnosis and appropriate treatment.
Maintaining good oral hygiene practices such as regular brushing, flossing, and dental check-ups can help prevent many oral infections. If you suspect you have an oral infection or are experiencing symptoms like persistent pain, swelling, or bleeding, it’s essential to consult a dentist or healthcare professional for proper diagnosis and treatment.
Most Common Oral Infections (Part 1)
Read this Article also – Vaginal Infections (Vaginitis, Vaginosis) Symptoms and Treatment
If you don’t like this article/post please share your feedback.