Migraine is a neurological disorder characterized by recurrent, throbbing headaches that typically affect one side of the head. Migraine headaches are often accompanied by other symptoms, such as nausea, vomiting, and sensitivity to light and sound. These headaches can be extremely debilitating and can last for several hours to several days, significantly impacting a person’s daily life.
Types of Migraine
There are several different types of migraines, each with its own characteristic features and symptoms.
The two most common types are:
- Migraine without Aura (formerly known as Common Migraine): This is the most common type of migraine. People with this type experience moderate to severe headache pain that is often one-sided and throbbing. They may also have associated symptoms such as nausea, vomiting, and sensitivity to light and sound. Migraine without aura does not involve the neurological symptoms known as auras.
- Migraine with Aura (formerly known as Classic Migraine): Some people with migraines experience auras before the onset of the headache. Auras are typically visual disturbances but can also involve other neurological symptoms. Visual auras may include flashing lights, zigzag lines, blind spots, or temporary loss of vision. Other aura symptoms can include tingling sensations in the face or hands, difficulty speaking, or confusion. After the aura phase, the headache typically follows.
Other less common types of migraines include:
- Chronic Migraine: This type of migraine is diagnosed when a person experiences a headache on 15 or more days per month for at least three months, and at least eight of those headaches are migraines. Chronic migraines can be extremely disabling.
- Menstrual Migraine: Some women experience migraines that are specifically triggered by hormonal changes associated with their menstrual cycle. These migraines typically occur in the days leading up to or during menstruation.
- Vestibular Migraine: Vestibular migraines are characterized by dizziness and problems with balance, in addition to typical migraine symptoms. These migraines can be particularly challenging to diagnose because they may not always include a severe headache.
- Retinal Migraine: Retinal migraines are rare and involve temporary vision loss or blindness in one eye. This vision loss is usually reversible but can be frightening.
- Hemiplegic Migraine: Hemiplegic migraines are extremely rare and cause temporary paralysis or weakness on one side of the body before or during the headache. Other symptoms can include difficulty speaking, confusion, and vision disturbances.
- Ocular Migraine: Ocular migraines cause temporary vision loss or disturbances in one eye. Unlike retinal migraines, ocular migraines affect both eyes but typically one at a time.
It’s important to note that migraine symptoms and types can vary from person to person, and some individuals may experience different types of migraines at different times. If you suspect you have migraines, it’s advisable to seek medical evaluation and guidance for proper diagnosis and management.
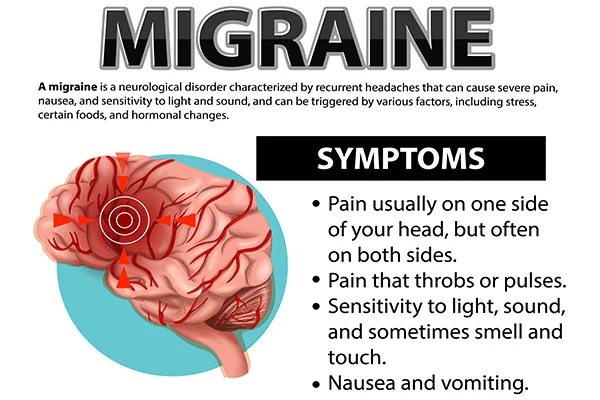
Symptoms of Migraine
Migraine symptoms can vary from person to person and can also differ in intensity and duration. The primary symptom of a migraine is a severe headache, typically accompanied by other symptoms.
Here are some common symptoms associated with migraines:
- Headache: Migraine headaches are often described as throbbing, pulsating, and intense. They usually affect one side of the head, but they can also be on both sides. The headache can last for several hours to several days.
- Aura (in some cases): Not all migraine sufferers experience auras, but for those who do, this is a distinctive symptom that occurs before or during the headache phase. Auras are usually visual disturbances but can also involve other neurological symptoms. Some common visual aura symptoms include seeing flashing lights, zigzag lines, blind spots, or temporary loss of vision. Other auras may involve tingling sensations in the face or hands, difficulty speaking, or confusion.
- Nausea and Vomiting: Many people with migraines experience nausea and may vomit during a migraine attack.
- Sensitivity to Light (Photophobia): Bright lights, sunlight, or even artificial light sources can worsen migraine symptoms and cause discomfort.
- Sensitivity to Sound (Phonophobia): Sounds, especially loud or repetitive noises, can be bothersome and increase pain during a migraine.
- Sensitivity to Smells (Osmophobia): Certain odors, even pleasant ones, can trigger or worsen migraine symptoms.
- Pain That Worsens With Physical Activity: Migraine pain is often exacerbated by routine physical activities, such as climbing stairs or bending over.
- Aura-Associated Symptoms (if present): Depending on the type of aura experienced, individuals may have symptoms such as tingling or numbness in the face or hands, difficulty speaking, confusion, or muscle weakness.
- Fatigue: After a migraine attack, individuals may feel extremely tired and drained.
- Difficulty Concentrating: Migraine attacks can impair cognitive function, making it difficult to concentrate or think clearly.
- Neck Pain: Some individuals with migraines experience neck pain or stiffness as part of their symptoms.
- Mood Changes: Migraines can lead to mood changes, such as irritability or feelings of depression and anxiety.
It’s important to note that not everyone with migraines experiences all of these symptoms, and the severity and frequency of symptoms can vary. Migraine symptoms can be disabling and have a significant impact on a person’s daily life. If you or someone you know is experiencing symptoms consistent with migraines, it’s important to seek medical evaluation and guidance for proper diagnosis and management.
Causes of Migraine
The exact cause of migraines is not fully understood, and they likely result from a combination of genetic, environmental, and neurological factors. Migraines are considered a complex neurological disorder.
Here are some of the key factors that are believed to contribute to the development of migraines:
- Genetics: Migraines often run in families, suggesting a genetic predisposition. If one or both of your parents have a history of migraines, you may be more likely to experience them.
- Neurological Factors: Migraines are thought to involve abnormal brain activity. It is believed that changes in the brain’s neurotransmitters, such as serotonin, play a role in triggering migraines. Serotonin levels drop during a migraine attack, which can contribute to blood vessel constriction and pain.
- Triggers: Migraine attacks can be triggered by a variety of factors, which can vary from person to person. Common triggers include:
– Certain foods and beverages, like aged cheeses, chocolate, caffeine, and alcohol.
– Skipping meals or fasting.
– Changes in sleep patterns or insufficient sleep.
– Stress and emotional factors.
– Hormonal fluctuations, such as those associated with menstruation, pregnancy, or menopause.
– Environmental factors, including changes in weather, strong smells, or exposure to bright lights and loud noises.
– Physical factors, like intense physical exertion, overexertion, or posture-related issues.
– Medications, including some oral contraceptives and certain blood pressure medications. - Hormonal Factors: Many women experience migraines that are closely linked to their menstrual cycles, known as menstrual migraines. Hormonal changes, particularly the drop in estrogen levels, can trigger these migraines.
- Vascular Changes: It was once believed that migraines were primarily caused by changes in blood vessel size and dilation in the brain. While vascular changes are still considered a factor, they are now understood to be part of a more complex process involving neurological and genetic factors.
- Serotonin Imbalance: Serotonin is a neurotransmitter that plays a role in regulating pain perception and mood. Fluctuations in serotonin levels can contribute to migraine attacks.
- Central Nervous System Sensitivity: Some researchers believe that individuals with migraines have a heightened sensitivity of their central nervous system to various triggers and stimuli.
- Inflammation: Inflammatory processes in the body may contribute to the development of migraines in some individuals.
It’s important to note that migraine triggers and causes can vary widely among individuals, and what may trigger a migraine in one person may not affect another. Additionally, the exact mechanisms underlying migraines are still an active area of research. Migraines are typically diagnosed based on their characteristic symptoms, and treatment approaches often focus on managing symptoms and preventing future attacks rather than addressing the root cause. If you experience migraines, it’s advisable to work with a healthcare professional to develop a personalized management plan.
Home Remedies of Migraine
While there is no cure for migraines, there are several home remedies and lifestyle changes that may help alleviate the severity and frequency of migraine attacks or provide relief during an episode. Keep in mind that what works can vary from person to person, and it’s essential to consult with a healthcare professional for a proper diagnosis and individualized treatment plan.
Here are some home remedies and strategies to consider:
- Identify and Avoid Triggers:
– Keep a migraine diary to track potential triggers like food, stress, sleep patterns, and environmental factors. Once identified, try to avoid or minimize exposure to these triggers. - Manage Stress:
– Practice relaxation techniques such as deep breathing, meditation, progressive muscle relaxation, or yoga to reduce stress, which can be a significant migraine trigger for many people. - Stay Hydrated:
– Dehydration can trigger migraines in some individuals. Make sure you’re drinking enough water throughout the day. - Regular Sleep Patterns:
– Maintain a consistent sleep schedule by going to bed and waking up at the same time every day, even on weekends. Avoid oversleeping. - Dietary Adjustments:
– Identify and avoid foods that may trigger migraines. Common culprits include aged cheeses, processed meats, chocolate, caffeine, and alcohol.
– Eat regular, balanced meals to avoid low blood sugar, which can trigger migraines. - Caffeine:
– Some people find relief from migraines by consuming a small amount of caffeine during an attack. However, excessive caffeine intake can lead to rebound headaches, so use it judiciously. - Ginger:
– Ginger has anti-inflammatory properties and may help relieve migraine symptoms. You can try ginger tea or ginger supplements. - Cold Compress:
– Apply a cold compress to your forehead or the back of your neck to help alleviate pain and reduce inflammation. - Rest in a Dark, Quiet Room:
– Sensitivity to light and sound is common during migraines. Find a dark, quiet room to rest and relax during an attack. - Aromatherapy:
– Some people find relief from migraines through aromatherapy. Lavender, peppermint, and eucalyptus oils are often used for their soothing effects. - Acupressure or Massage:
– Gentle massage or acupressure on specific points, such as the temples or the space between the thumb and index finger, may provide relief. - Hydrate with Electrolyte Drinks:
– If nausea and vomiting are present during a migraine attack, consider hydrating with electrolyte drinks or ice chips. - Biofeedback and Relaxation Training:
– These techniques can help you learn to control certain bodily functions and reduce the frequency and severity of migraines. - Supplements:
– Some supplements, such as magnesium, riboflavin (vitamin B2), and coenzyme Q10, have been studied for their potential to reduce migraine frequency.
It’s important to remember that while these home remedies may provide relief for some individuals, they may not work for everyone. If your migraines are severe, frequent, or significantly affect your daily life, consult a healthcare professional for a proper diagnosis and a personalized treatment plan, which may include medications or other medical interventions to manage your condition effectively.
When do migraines start?
Migraines can start at any age, but they often begin in adolescence or early adulthood. However, they can also develop later in life. The age at which migraines first appear varies from person to person. Some individuals experience their first migraine attack as children, while others may not have their first migraine until their 30s, 40s, or later.
Migraines can continue throughout a person’s life once they start, but the frequency, severity, and triggers of migraine attacks can change over time. In some cases, migraines may become less frequent or severe as a person gets older, while in others, they may persist or worsen.
It’s important to note that migraines can be hereditary, meaning they may run in families. If you have a family history of migraines, you may be more likely to develop them at some point in your life.
If you experience symptoms that you suspect are migraines or if you have concerns about headaches or head pain, it’s advisable to consult with a healthcare professional. They can help diagnose your condition, provide appropriate treatment options, and offer guidance on managing your migraines effectively.
Why do people get migraines?
The exact cause of migraines is not fully understood, but they are believed to result from a combination of genetic, environmental, and neurological factors. Migraines are considered a complex neurological disorder.
Here are some key factors that are thought to contribute to the development of migraines:
- Genetics: Migraines often run in families, suggesting a genetic predisposition. If one or both of your parents have a history of migraines, you may be more likely to experience them.
- Neurological Factors: Migraines are thought to involve abnormal brain activity. Changes in the brain’s neurotransmitters, such as serotonin, play a role in triggering migraines. Serotonin levels drop during a migraine attack, which can contribute to blood vessel constriction and pain.
- Triggers: Migraine attacks can be triggered by a variety of factors, which can vary from person to person. Common triggers include:
– Certain foods and beverages, like aged cheeses, chocolate, caffeine, and alcohol.
– Skipping meals or fasting.
– Changes in sleep patterns or insufficient sleep.
– Stress and emotional factors.
– Hormonal fluctuations, such as those associated with menstruation, pregnancy, or menopause.
– Environmental factors, including changes in weather, strong smells, or exposure to bright lights and loud noises.
– Physical factors, like intense physical exertion, overexertion, or posture-related issues.
– Medications, including some oral contraceptives and certain blood pressure medications. - Hormonal Factors: Many women experience migraines that are closely linked to their menstrual cycles, known as menstrual migraines. Hormonal changes, particularly the drop in estrogen levels, can trigger these migraines.
- Vascular Changes: While once believed to be the primary cause, vascular changes in the brain are now considered part of a more complex process. These changes may include blood vessel constriction followed by dilation, which can contribute to migraine pain.
- Serotonin Imbalance: Serotonin is a neurotransmitter that plays a role in regulating pain perception and mood. Fluctuations in serotonin levels can contribute to migraine attacks.
- Central Nervous System Sensitivity: Some researchers believe that individuals with migraines have a heightened sensitivity of their central nervous system to various triggers and stimuli.
- Inflammation: Inflammatory processes in the body may contribute to the development of migraines in some individuals.
It’s important to note that migraine triggers and causes can vary widely among individuals, and what may trigger a migraine in one person may not affect another. Additionally, the exact mechanisms underlying migraines are still an active area of research. Migraines are typically diagnosed based on their characteristic symptoms, and treatment approaches often focus on managing symptoms and preventing future attacks rather than addressing the root cause. If you experience migraines, it’s advisable to work with a healthcare professional to develop a personalized management plan.
Understanding Syncope: Symptoms, Causes & Home Remedies
Freckle: Symptoms, Causes, Prevention & Need to Know
Dehydration: Symptoms, Causes, & You Should Know About
Stress: Symptoms, Causes & Prevention
Snoring: Types, Symptoms, Causes & Home Remedies
Epilepsy: Symptoms, Causes & Home Remedies
Alzheimer’s Disease: Symptoms, Causes, & Prevention
Respiratory Disease: Symptoms, Causes, Preventive & Remedies
Iodine Deficiency: Symptoms, Causes, & Home Remedies
Insomnia: Types, Symptoms, Causes & Prevention
Sunburn: Symptoms, Causes, Prevention & Home Remedies
Sore Throat, Symptoms, Causes, Prevention & Home Remedies
Dandruff: Types, Symptoms, Causes & Prevention
Dark Circles Under Eyes: Symptoms, Remedies & Prevention
Heart Attack: Types, Symptoms & Prevention
Eye Infections: Symptoms, Causes & Treatment
Vertigo: Causes, Symptoms, Treatment & Preventive
Hair Loss, Types, Symptoms, Prevention & Treatments
Knee Pain, Symptoms, Types & Self Management
If you don’t like this article/post please share your feedback