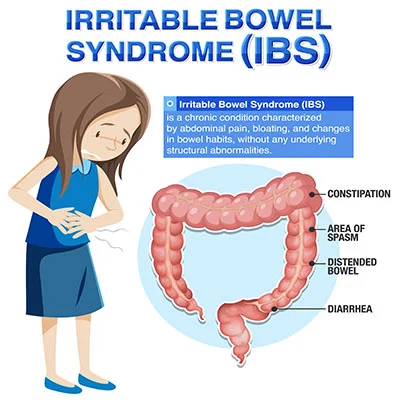
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder that affects the functioning of the digestive system. It is a chronic condition characterized by a group of symptoms related to the colon (large intestine) and can cause discomfort and disruption in a person’s daily life. IBS is a functional disorder, which means there is no structural or physical damage to the digestive tract, but rather, it is a disorder of how the digestive system functions.
Types of Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is typically categorized into several subtypes based on the predominant bowel habits and symptoms that a person experiences. The Rome criteria, which are widely used in diagnosing and classifying IBS, define these subtypes.
The primary IBS subtypes include:
- IBS with Constipation (IBS-C):
– In this subtype, individuals primarily experience constipation as a dominant symptom.
– Common symptoms include infrequent bowel movements, hard and lumpy stools, and a sensation of incomplete evacuation. - IBS with Diarrhea (IBS-D):
– IBS-D is characterized by frequent episodes of diarrhea as the main symptom.
– People with IBS-D may have loose or watery stools, urgency to have bowel movements, and may experience abdominal pain or discomfort. - Mixed IBS (IBS-M):
– This subtype is also known as IBS-Mixed, and individuals with IBS-M experience a combination of both diarrhea and constipation.
– Symptoms may alternate between constipation and diarrhea, often with abdominal discomfort. - Unsubtyped IBS (IBS-U):
– Some individuals may not fit clearly into one of the specific subtypes, or their symptoms may fluctuate between different subtypes over time. These cases are categorized as IBS-U, which stands for “unsubtyped.”
In addition to these primary subtypes, some experts also recognize a subtype called Post-Infectious IBS (PI-IBS). PI-IBS develops after a severe gastrointestinal infection (gastroenteritis) and is characterized by IBS symptoms that occur following the infection. It can manifest as either diarrhea-predominant or constipation-predominant.
It’s important to note that IBS is a complex and heterogeneous condition, and individuals may experience a wide range of symptoms and variations in severity. The classification into subtypes is primarily for clinical purposes to help guide treatment approaches. Many people with IBS may also have additional symptoms such as abdominal pain or bloating, and these can occur across all subtypes.
Treatment for IBS depends on the predominant symptoms and may involve dietary changes, stress management, lifestyle modifications, and medications tailored to address specific symptoms. It’s essential for individuals with IBS to work closely with a healthcare provider to develop a personalized treatment plan based on their specific subtype and symptom profile.
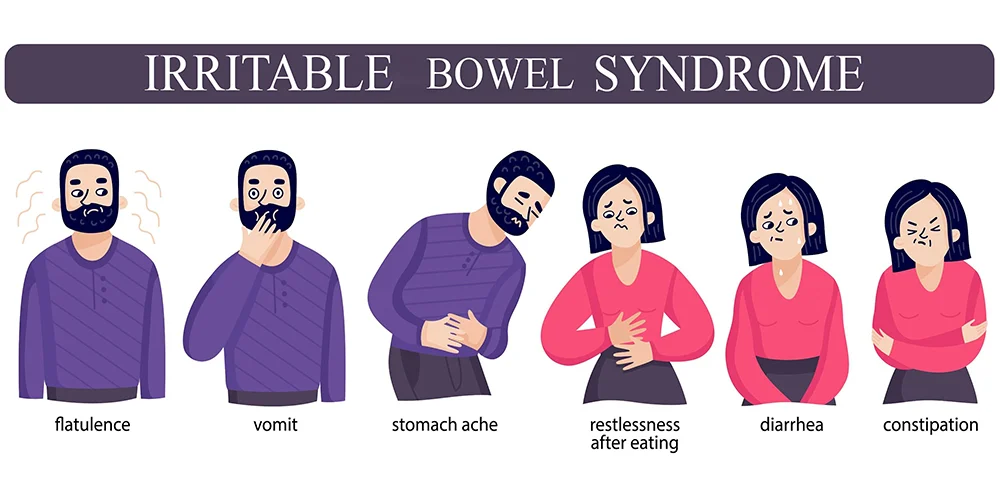
Symptoms of Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) can manifest with a variety of symptoms, and the severity and combination of these symptoms can vary from person to person.
The most common symptoms of IBS include:
- Abdominal Pain or Discomfort:
– IBS often presents with recurrent and crampy abdominal pain or discomfort. This pain is typically located in the lower abdomen and may be relieved after a bowel movement. - Altered Bowel Habits:
– IBS can lead to changes in bowel habits, and these changes are often a defining feature of the condition. The primary altered bowel habits associated with IBS include:
– Diarrhea (IBS-D): Frequent, loose, or watery stools.
– Constipation (IBS-C): Infrequent bowel movements, often with hard and lumpy stools.
– Mixed Bowel Habits (IBS-M): Alternating between episodes of diarrhea and constipation. - Bloating and Gas:
– Many people with IBS experience excessive gas production and abdominal bloating, leading to feelings of fullness and discomfort. - Urgency:
– People with IBS may have a sudden and strong urge to have a bowel movement, often leading to a need to rush to the restroom. - Changes in Stool Appearance:
– Stools in IBS can vary in appearance and consistency. Some individuals may notice changes such as mucus in the stool, which is not typically present in healthy stools. - Incomplete Evacuation:
– Some individuals with IBS may feel that they haven’t completely emptied their bowels after a bowel movement. - Increased Bowel Movements:
– IBS can lead to an increase in the frequency of bowel movements, which can be especially prominent in the diarrhea-predominant subtype (IBS-D). - Fatigue:
– Chronic IBS symptoms can be physically and emotionally draining, leading to feelings of fatigue. - Anxiety and Depression:
– Psychological symptoms such as anxiety and depression are more common in individuals with IBS, and these conditions can sometimes exacerbate IBS symptoms.
It’s important to note that IBS is a functional gastrointestinal disorder, meaning there is no structural abnormality or damage in the digestive tract that can be identified through standard medical tests. Diagnosis is typically based on the presence of characteristic symptoms, and healthcare providers may use the Rome criteria to help confirm the diagnosis.
The severity and duration of IBS symptoms can vary widely, and they may be influenced by factors such as diet, stress, hormonal fluctuations, and other individual triggers. Managing IBS often involves a combination of dietary modifications, lifestyle changes, stress management, and, in some cases, medications to alleviate specific symptoms. If you suspect you have IBS or are experiencing persistent gastrointestinal symptoms, it is advisable to consult a healthcare professional for proper evaluation and guidance.
Causes of Irritable Bowel Syndrome
The exact cause of Irritable Bowel Syndrome (IBS) is not fully understood, and it is likely to result from a combination of factors. IBS is considered a multifactorial condition, and several potential contributors have been identified.
Some of the key factors believed to play a role in the development of IBS include:
- Abnormal Gastrointestinal Motility: One of the leading theories regarding the cause of IBS is abnormal gastrointestinal motility. This refers to irregular contractions of the muscles in the digestive tract, which can lead to symptoms like diarrhea or constipation in IBS-D and IBS-C subtypes, respectively.
- Visceral Hypersensitivity: Many individuals with IBS have heightened sensitivity to pain and discomfort in their gastrointestinal tract. Even normal contractions of the intestines can be perceived as painful or uncomfortable in individuals with visceral hypersensitivity.
- Altered Gut Microbiota: Research has shown that the composition and activity of the gut microbiota (the community of microorganisms living in the intestines) can play a role in IBS. Changes in the balance of beneficial and harmful bacteria in the gut may contribute to IBS symptoms.
- Food Sensitivities and Diet: Certain foods and dietary factors can trigger or exacerbate IBS symptoms in some individuals. Common triggers include certain carbohydrates (FODMAPs), fatty foods, caffeine, alcohol, and artificial sweeteners.
- Stress and Psychological Factors: Stress and psychological factors, such as anxiety and depression, can influence the onset and severity of IBS symptoms. The gut-brain connection is well-established, and emotional stress can exacerbate gastrointestinal symptoms.
- Infections and Post-Infectious IBS: Some cases of IBS develop after a gastrointestinal infection, a condition known as Post-Infectious IBS (PI-IBS). The infection can lead to long-lasting changes in gut function and trigger IBS symptoms.
- Hormonal Changes: Hormonal fluctuations, particularly in women, can influence IBS symptoms. Some women experience changes in symptoms during their menstrual cycle, and hormonal factors may play a role in the gender disparity observed in IBS cases.
- Genetic Factors: While no specific gene has been identified as the sole cause of IBS, there is evidence to suggest a genetic predisposition in some individuals. A family history of IBS may increase the risk of developing the condition.
It’s important to note that IBS is a complex and heterogeneous condition, and the specific causes and triggers can vary from person to person. Additionally, IBS is diagnosed based on the presence of characteristic symptoms and the exclusion of other gastrointestinal conditions. There is no single diagnostic test for IBS, so healthcare providers often rely on clinical evaluation and symptom patterns to make a diagnosis.
Treatment for IBS typically focuses on managing symptoms and addressing contributing factors. This may involve dietary modifications, stress management techniques, lifestyle changes, and medications to alleviate specific symptoms. Individualized treatment plans are often necessary, as what works for one person with IBS may not be effective for another. Consulting a healthcare professional is essential for proper evaluation and guidance in managing IBS symptoms.
Prevention of Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is a complex and multifactorial condition, and while there is no known way to completely prevent it, there are strategies that may help reduce the risk of developing or exacerbating IBS symptoms in susceptible individuals.
Here are some tips for potential prevention and symptom management:
- Dietary Modifications:
– Pay attention to your diet, as certain foods can trigger IBS symptoms. Consider keeping a food diary to identify specific triggers and then try to avoid or limit those foods.
– Some people with IBS find relief by following a low-FODMAP diet, which reduces the intake of certain carbohydrates that can ferment in the gut and cause symptoms.
– Eating smaller, more frequent meals instead of large ones can help prevent overloading the digestive system. - Stress Management:
– Chronic stress can exacerbate IBS symptoms. Practice stress reduction techniques such as deep breathing exercises, meditation, yoga, or mindfulness to help manage stress.
– Regular physical activity can also be effective in reducing stress and improving overall well-being. - Balanced Lifestyle:
– Aim for a balanced lifestyle with regular sleep patterns. Poor sleep can contribute to digestive disturbances and worsen IBS symptoms.
– Limit alcohol and caffeine consumption, as these substances can irritate the gastrointestinal tract. - Hydration:
– Staying adequately hydrated is important for digestive health. Drink plenty of water throughout the day. - Fiber Intake:
– For some individuals, increasing dietary fiber can help regulate bowel movements and alleviate symptoms. However, for others, excessive fiber intake may exacerbate symptoms. It’s essential to work with a healthcare provider to determine the right amount and type of fiber for your specific case. - Probiotics:
– Probiotics are beneficial bacteria that can promote gut health. Some people with IBS find relief from certain probiotic supplements. Consult with a healthcare provider before starting any probiotic regimen. - Regular Exercise:
– Engaging in regular physical activity can help maintain healthy bowel function and reduce stress. - Avoid Smoking:
– If you smoke, consider quitting. Smoking is associated with an increased risk of IBS. - Medication Use:
– Use medications, including antibiotics and over-the-counter pain relievers, only as directed by a healthcare provider, as some medications can irritate the gastrointestinal tract. - Seek Professional Guidance:
– If you suspect you have IBS or are experiencing persistent gastrointestinal symptoms, consult a healthcare professional. They can provide a proper diagnosis and work with you to develop a personalized treatment plan.
It’s important to note that what works to prevent or manage IBS can vary from person to person. IBS is a complex condition with diverse triggers and symptom profiles. Therefore, it’s crucial to work closely with a healthcare provider to determine the most appropriate strategies for your specific case and to rule out other potential underlying medical conditions.
How can IBS affect daily life?
Irritable Bowel Syndrome (IBS) can significantly impact a person’s daily life due to the chronic and often unpredictable nature of its symptoms. The severity of IBS symptoms varies from person to person, but for many individuals,
IBS can have a range of effects on their daily routines and quality of life, including:
- Discomfort and Pain: The abdominal pain and discomfort associated with IBS can be disruptive. It may range from mild to severe and can occur suddenly, leading to interruptions in daily activities.
- Altered Bowel Habits: Frequent episodes of diarrhea or constipation, or a combination of both, can require frequent trips to the restroom, which can be inconvenient and disruptive.
- Urgency: The sudden and strong urge to have a bowel movement can be distressing and may necessitate quick access to a restroom.
- Social and Emotional Impact: IBS can lead to anxiety and embarrassment, as individuals may worry about having symptoms in public or social settings. Socializing and participating in events may become more challenging.
- Work and Productivity: IBS symptoms can affect work and productivity. Frequent restroom breaks, time away from work due to symptoms, or the need for flexible work arrangements can impact job performance and career advancement.
- Dietary Restrictions: Many people with IBS must make dietary modifications to manage their symptoms. This can involve avoiding specific foods or following special diets, which may limit food choices and affect social dining experiences.
- Psychological Well-Being: The chronic nature of IBS can lead to stress, anxiety, and depression. The psychological impact of the condition can worsen symptoms, creating a vicious cycle.
- Fatigue: Dealing with chronic symptoms and discomfort can be exhausting, leading to fatigue and reduced energy levels.
- Impact on Relationships: IBS can affect personal relationships, as individuals may need to explain their condition to others and may face challenges in maintaining social and intimate relationships.
- Medical Expenses: The costs associated with doctor visits, diagnostic tests, and medications can add up over time.
- Limitations on Activities: Some people with IBS may avoid certain activities or situations due to fear of symptoms occurring, leading to a reduced quality of life.
- Isolation: In severe cases, individuals with IBS may become socially isolated, withdrawing from friends and family due to the unpredictable nature of their symptoms.
It’s important to note that while IBS can have a significant impact on daily life, it is a manageable condition. Many people with IBS find relief through dietary modifications, stress management, medications, and lifestyle adjustments. Seeking medical advice and working with healthcare providers to develop a personalized treatment plan can help individuals with IBS better manage their symptoms and improve their overall quality of life. Additionally, seeking support from support groups or mental health professionals can be valuable in addressing the emotional and psychological aspects of living with IBS.
Can IBS be treated with diet?
Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder characterized by symptoms such as abdominal pain, bloating, gas, and changes in bowel habits, such as diarrhea or constipation. While there is no known cure for IBS, Dietary changes can often help manage and alleviate its symptoms for many individuals.
Here are some dietary approaches that may be helpful in managing IBS:
- Low-FODMAP Diet: FODMAPs are certain types of carbohydrates that can trigger IBS symptoms in some people. A low-FODMAP diet involves avoiding high-FODMAP foods like certain fruits, vegetables, dairy products, and grains. This approach should be done under the guidance of a healthcare professional or registered dietitian as it is restrictive and not suitable for long-term use.
- High-Fiber Diet: Some people with IBS, especially those with constipation-predominant IBS, may benefit from a high-fiber diet. Soluble fiber, in particular, can help regulate bowel movements and reduce symptoms. Foods like oats, psyllium, and certain fruits and vegetables are good sources of soluble fiber.
- Probiotics: Probiotics are live microorganisms that can help improve gut health. Some IBS patients find relief from symptoms by taking specific strains of probiotics. However, the effectiveness of probiotics can vary from person to person, and it’s best to consult a healthcare provider before starting any probiotic regimen.
- Avoid Trigger Foods: Many individuals with IBS have specific trigger foods that worsen their symptoms. Common triggers include spicy foods, fatty foods, caffeine, alcohol, and artificial sweeteners. Keeping a food diary can help identify and avoid these triggers.
- Regular Meal Patterns: Eating regular, balanced meals and not skipping meals can help stabilize digestion and reduce symptoms in some people.
- Hydration: Drinking plenty of water is important for overall digestive health and can help alleviate symptoms.
It’s crucial to note that the effectiveness of dietary changes in managing IBS can vary from person to person. What works for one individual may not work for another. It’s also important to rule out other potential causes of gastrointestinal symptoms, so if you suspect you have IBS or are experiencing digestive issues, it’s advisable to consult a healthcare provider or a registered dietitian who can provide personalized guidance and recommendations based on your specific symptoms and needs. They can help you develop a suitable dietary plan to manage your IBS symptoms effectively.
Breast Cancer: Types, Symptoms, Causes, & Prevention
Migraine: Types, Symptoms, Causes & Home Remedies
Understanding Syncope: Symptoms, Causes & Home Remedies
Freckle: Symptoms, Causes, Prevention & Need to Know
Dehydration: Symptoms, Causes, & You Should Know About
Stress: Symptoms, Causes & Prevention
Snoring: Types, Symptoms, Causes & Home Remedies
Epilepsy: Symptoms, Causes & Home Remedies
Alzheimer’s Disease: Symptoms, Causes, & Prevention
Respiratory Disease: Symptoms, Causes, Preventive & Remedies
Iodine Deficiency: Symptoms, Causes, & Home Remedies
Insomnia: Types, Symptoms, Causes & Prevention
Sunburn: Symptoms, Causes, Prevention & Home Remedies
Sore Throat, Symptoms, Causes, Prevention & Home Remedies
Dandruff: Types, Symptoms, Causes & Prevention
Dark Circles Under Eyes: Symptoms, Remedies & Prevention
Heart Attack: Types, Symptoms & Prevention
Eye Infections: Symptoms, Causes & Treatment
Vertigo: Causes, Symptoms, Treatment & Preventive
Hair Loss, Types, Symptoms, Prevention & Treatments
Knee Pain, Symptoms, Types & Self Management
If you don’t like this article/post please share your feedback