Insomnia: is a sleep disorder characterized by the difficulty of falling asleep, staying asleep, or obtaining restful sleep, despite having the opportunity to do so. It often leads to daytime symptoms such as fatigue, irritability, difficulty concentrating, and impaired functioning. Insomnia can be either short-term (acute) or ongoing (chronic), and its causes can vary from stress and lifestyle factors to medical conditions and medications. Effective management of insomnia typically involves identifying and addressing its underlying triggers, adopting healthy sleep habits, and sometimes utilizing medical or therapeutic interventions.
Types of Insomnia
Insomnia can be categorized into different types based on its duration, underlying causes, and characteristics.
Here are some common types of insomnia:
- Acute Insomnia: This is a short-term type of insomnia that typically lasts for a few nights to a few weeks. It is often triggered by specific life events or stressors, such as an upcoming exam, work-related pressures, travel, or personal issues. Acute insomnia usually resolves once the triggering factors are resolved or managed.
- Chronic Insomnia: This type of insomnia persists for an extended period, generally for at least three nights a week for three months or more. Chronic insomnia is often related to underlying medical conditions, psychological factors, or long-term stress. It can significantly affect a person’s overall well-being.
- Onset Insomnia: This refers to difficulty falling asleep at the beginning of the night. Individuals with onset insomnia may spend a prolonged time trying to initiate sleep, even when they feel physically tired.
- Maintenance Insomnia: People with maintenance insomnia have trouble staying asleep during the night. They may wake up multiple times during the night and struggle to return to sleep, leading to fragmented and non-restorative sleep.
- Comorbid Insomnia: This type of insomnia occurs alongside other medical or psychiatric conditions. For instance, insomnia is often seen in conjunction with conditions like depression, anxiety, chronic pain, and certain medical disorders. Treating the underlying condition may help improve insomnia symptoms.
- Behavioral Insomnia of Childhood: This term is used to describe sleep difficulties in children that arise from behavioral factors, such as bedtime resistance, refusal to go to bed, or difficulty staying in their own bed throughout the night.
- Psychophysiology Insomnia: This type of insomnia often starts with an initial stressful event, like a difficult life transition. Over time, the worry about sleep itself becomes a major contributor to ongoing sleep difficulties, creating a cycle of anxiety and poor sleep.
- Idiopathic Insomnia: This is a rare type of insomnia that typically begins in childhood and persists into adulthood. It is thought to have a genetic basis and is characterized by a lifelong struggle to obtain adequate sleep, regardless of external factors.
- Paradoxical Insomnia (Sleep State Misperception): People with this type of insomnia believe they are getting very little sleep, even though objective measures show that they are sleeping more than they perceive. It’s a discrepancy between their perception of sleep and the actual amount of sleep obtained.
- Medical or Secondary Insomnia: Some medical conditions, medications, or substances can lead to insomnia as a secondary symptom. Conditions like chronic pain, asthma, acid reflux, and medications such as certain antidepressants or stimulants can interfere with sleep.
These types of insomnia can often overlap, and a thorough evaluation by a healthcare professional is necessary to determine the underlying causes and appropriate treatment strategies.
Symptoms of Insomnia
The symptoms of insomnia can vary in their intensity and duration, depending on the type and underlying causes of the condition.
Common symptoms of insomnia include:
- Difficulty Falling Asleep: Individuals with insomnia may find it challenging to fall asleep at bedtime, even when they feel physically tired.
- Frequent Waking: People with insomnia often wake up multiple times during the night and have difficulty returning to sleep. These awakenings can lead to fragmented sleep.
- Waking Up Too Early: Some individuals with insomnia wake up earlier than desired and are unable to go back to sleep. This can result in not getting enough total sleep time.
- Non-Restorative Sleep: Even if individuals with insomnia manage to sleep, they might wake up feeling unrefreshed and still tired.
- Daytime Fatigue: Insomnia can lead to significant daytime sleepiness and fatigue, which can affect daily functioning, work performance, and overall quality of life.
- Difficulty Concentrating: Insomnia can impair cognitive functions such as concentration, memory, and decision-making, making it challenging to perform tasks effectively.
- Irritability and Mood Disturbances: Lack of sleep can contribute to irritability, mood swings, increased sensitivity to stress, and even heightened emotional responses.
- Anxiety About Sleep: People with insomnia may develop anxiety about their ability to fall asleep or stay asleep, which can further exacerbate the sleep difficulties.
- Physical Symptoms: Insomnia can lead to physical symptoms such as headaches, gastrointestinal discomfort, and muscle tension.
- Depression: Chronic insomnia is closely linked to an increased risk of developing or exacerbating mood disorders, such as depression and anxiety.
- Tension and Worry: Individuals with insomnia often spend a significant amount of time worrying about their sleep and the potential consequences of not getting enough rest.
- Increased Use of Sleep Aids: In an attempt to manage their sleep problems, some people with insomnia might rely on over-the-counter sleep aids or prescription medications, which may or may not be effective in the long term.
It’s important to note that occasional sleep difficulties are common and do not necessarily indicate insomnia. Insomnia is diagnosed when these symptoms are persistent and interfere with daily functioning. If you or someone you know is experiencing ongoing sleep problems that impact their well-being, it’s advisable to consult a healthcare professional for a proper evaluation and guidance on managing the condition.
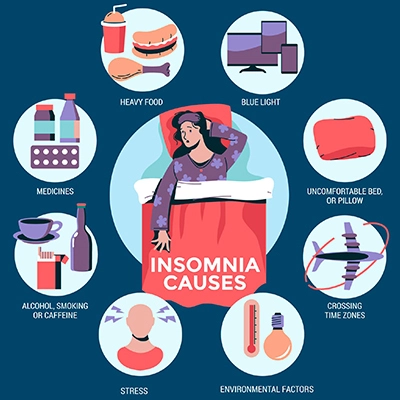
Causes of Insomnia
Insomnia can be caused by a variety of factors, which can be grouped into several categories. Often, it’s a combination of these factors that contribute to the development of insomnia.
Some common causes of insomnia include:
- Stress and Anxiety: Mental and emotional stress, such as worries about work, family, finances, or personal issues, can make it difficult to relax and fall asleep. Anxiety disorders can also directly contribute to insomnia.
- Depression: Depression is often linked to sleep disturbances. It can lead to difficulty falling asleep, waking up early, or experiencing non-restorative sleep.
- Poor Sleep Hygiene: Unhealthy sleep habits, such as irregular sleep schedules, excessive daytime napping, and using electronic devices before bed, can disrupt the body’s natural sleep-wake cycle and lead to insomnia.
- Medical Conditions: Chronic pain conditions (like arthritis or fibromyalgia), respiratory disorders (such as asthma), gastrointestinal issues (like acid reflux), and hormonal imbalances (such as thyroid problems) can all contribute to insomnia.
- Medications: Some medications, such as certain antidepressants, stimulants, and medications for high blood pressure or asthma, can interfere with sleep patterns and lead to insomnia.
- Substance Use: The consumption of caffeine, nicotine, and alcohol, particularly close to bedtime, can disrupt sleep. While alcohol might initially make a person feel drowsy, it can lead to fragmented sleep later in the night.
- Environmental Factors: Noisy or uncomfortable sleep environments, changes in time zones due to travel (jet lag), and working night shifts can disrupt sleep patterns and lead to insomnia.
- Circadian Rhythm Disorders: Disorders like shift work sleep disorder and delayed sleep phase disorder can cause a mismatch between a person’s natural body clock and their desired sleep schedule.
- Behavioral Factors: Associating the bed with activities other than sleep (like working or watching TV), irregular sleep schedules, and excessive worrying about sleep can all contribute to insomnia.
- Age: As people age, they may experience changes in their sleep patterns and hormone levels that can make it more difficult to get a good night’s sleep.
- Hormonal Changes: Hormonal fluctuations, such as those that occur during pregnancy or menopause, can lead to sleep disturbances and insomnia.
- Psychophysiology Factors: This term refers to the cycle of worrying about sleep itself, which can lead to heightened anxiety and make it even more difficult to fall asleep.
- Genetic Factors: Some individuals may have a genetic predisposition to insomnia or sleep disturbances.
It’s important to note that identifying the underlying causes of insomnia is crucial for effective treatment. If insomnia is persistent and significantly impacting your quality of life, seeking guidance from a healthcare professional, such as a primary care physician or a sleep specialist, is recommended to determine the appropriate course of action.

Prevention of Insomnia
While it’s not always possible to completely prevent insomnia, there are several steps you can take to reduce your risk of developing sleep problems and improve your sleep quality.
Here are some tips for preventing insomnia:
- Maintain a Consistent Sleep Schedule: Go to bed and wake up at the same times every day, even on weekends. This helps regulate your body’s internal clock and promotes better sleep.
- Create a Relaxing Bedtime Routine: Establish calming pre-sleep activities like reading, listening to soothing music, or practicing relaxation techniques to signal to your body that it’s time to wind down.
- Create a Comfortable Sleep Environment: Ensure that your bedroom is conducive to sleep. Keep the room dark, quiet, and at a comfortable temperature. Use a comfortable mattress and pillows.
- Limit Exposure to Screens Before Bed: The blue light emitted by phones, tablets, computers, and TVs can interfere with your body’s production of melatonin, a hormone that helps regulate sleep. Try to avoid screens for at least an hour before bedtime.
- Limit Stimulants and Alcohol: Reduce your intake of caffeine and nicotine, especially in the afternoon and evening. While alcohol might initially make you feel drowsy, it can disrupt sleep later in the night.
- Avoid Heavy Meals Before Bed: Eating a large, heavy meal close to bedtime can lead to discomfort and indigestion, making it harder to fall asleep.
- Stay Active During the Day: Regular physical activity can improve sleep quality. Aim for at least 30 minutes of exercise most days, but avoid vigorous exercise close to bedtime.
- Manage Stress and Anxiety: Practice stress-reduction techniques such as deep breathing, meditation, yoga, or progressive muscle relaxation to manage anxiety and promote relaxation.
- Limit Daytime Naps: While short naps can be refreshing, long or irregular daytime naps can disrupt your nighttime sleep. If you need to nap, keep it under 30 minutes and earlier in the day.
- Limit Liquid Intake Before Bed: Minimize the consumption of fluids in the evening to reduce the likelihood of waking up for bathroom trips during the night.
- Manage Your Worries: If racing thoughts are keeping you awake, consider setting aside time during the day to address your concerns, so they’re not as likely to keep you up at night.
- Evaluate Your Medications: If you suspect that certain medications might be affecting your sleep, consult your healthcare provider to discuss possible alternatives or adjustments.
- Expose Yourself to Natural Light: Natural light exposure during the day helps regulate your body’s internal clock. Spend time outdoors or open your curtains during the day.
- Limit Clock-Watching: Constantly checking the clock during the night can create anxiety about sleep. If you wake up during the night, avoid looking at the clock.
- Seek Professional Help: If you’re experiencing persistent sleep difficulties or insomnia, consider consulting a healthcare professional. They can help identify underlying causes and recommend appropriate treatments.
Remember that everyone’s sleep needs are different, and it might take some trial and error to find the strategies that work best for you. If your sleep problems persist, seeking guidance from a healthcare provider, particularly a sleep specialist, can provide personalized advice and solutions.
How does insomnia start?
Insomnia can start for a variety of reasons, and its onset can be triggered by a combination of factors.
Here are some common scenarios that can lead to the development of insomnia:
- Stressful Life Events: Major life events such as relationship issues, work-related pressures, financial problems, loss of a loved one, or other sources of stress can trigger acute insomnia. The stress and emotional turmoil from these events can make it difficult for your mind to relax, leading to sleep difficulties.
- Poor Sleep Habits: Adopting unhealthy sleep habits, such as irregular sleep schedules, excessive napping during the day, and engaging in stimulating activities (like watching intense movies or using electronic devices) close to bedtime, can disrupt your body’s natural sleep-wake cycle and lead to difficulty falling asleep.
- Underlying Medical Conditions: Physical health issues such as chronic pain conditions (e.g., arthritis), respiratory problems (e.g., asthma), gastrointestinal disorders (e.g., acid reflux), or hormonal imbalances can cause discomfort that makes it hard to sleep through the night.
- Mental Health Conditions: Disorders like anxiety, depression, and post-traumatic stress disorder (PTSD) can lead to heightened arousal, excessive rumination, and overall psychological distress, all of which can interfere with falling asleep and staying asleep.
- Medications: Certain medications, especially stimulants (e.g., some medications for attention-deficit/hyperactivity disorder) or medications that affect the central nervous system (e.g., certain antidepressants), can disrupt sleep patterns and cause insomnia.
- Substance Use: Consuming substances like caffeine, nicotine, and alcohol, particularly close to bedtime, can interfere with sleep. While alcohol might initially make you feel sleepy, it can lead to fragmented sleep later in the night.
- Shift Work or Jet Lag: Sudden changes in your sleep schedule due to shift work or traveling across multiple time zones can disrupt your body’s internal clock, leading to difficulty falling asleep and staying asleep.
- Aging: As people age, changes in sleep patterns, hormone levels, and health conditions can lead to increased susceptibility to sleep disturbances, including insomnia.
- Pre-existing Sleep Disorders: Conditions like sleep apnea, restless legs syndrome, and narcolepsy can cause disruptions in sleep and contribute to insomnia.
- Psychophysiology Factors: In some cases, the initial cause of insomnia might be a stressful event or situation, but over time, the anxiety and worry about sleep itself become a major contributor to ongoing sleep difficulties.
It’s important to recognize that insomnia can be caused by a combination of factors, and pinpointing the exact cause might not always be straightforward. If you find yourself experiencing persistent sleep difficulties, it’s a good idea to consult a healthcare professional. They can help identify potential triggers and recommend appropriate strategies to improve your sleep.
How do I end insomnia?
Ending insomnia often requires a combination of lifestyle changes, behavioral adjustments, and sometimes professional intervention. Keep in mind that results may not be immediate, and it might take some time to establish new habits and see improvements in your sleep.
Here are some steps you can take to work towards overcoming insomnia:
- Establish a Consistent Sleep Schedule: Go to bed and wake up at the same times every day, even on weekends. This helps regulate your body’s internal clock.
- Create a Relaxing Bedtime Routine: Engage in calming activities before bed, such as reading, listening to soothing music, taking a warm bath, or practicing relaxation techniques.
- Create a Comfortable Sleep Environment: Ensure your bedroom is conducive to sleep by keeping it dark, quiet, and at a comfortable temperature. Use comfortable bedding and consider using blackout curtains if necessary.
- Limit Screen Time Before Bed: Reduce exposure to screens (phones, tablets, computers, TVs) at least an hour before bedtime to avoid the disruption of melatonin production.
- Limit Stimulants and Alcohol: Reduce or eliminate caffeine and nicotine intake, especially in the afternoon and evening. Limit alcohol consumption, particularly closer to bedtime.
- Engage in Regular Physical Activity: Regular exercise can improve sleep quality. Aim for at least 30 minutes of moderate exercise most days, but avoid vigorous activity close to bedtime.
- Practice Stress Management: Engage in stress-reduction techniques such as deep breathing, meditation, progressive muscle relaxation, or yoga to manage anxiety and promote relaxation.
- Improve Sleep Hygiene: Adopt healthy sleep habits like avoiding heavy meals before bedtime, limiting daytime naps, and keeping your bedroom reserved for sleep and intimacy only.
- Limit Liquid Intake Before Bed: Minimize the consumption of fluids in the evening to reduce the likelihood of waking up for bathroom trips during the night.
- Manage Worries: Set aside time during the day to address concerns or worries, so they’re less likely to keep you up at night.
- Limit Clock-Watching: Avoid constantly checking the clock during the night, as it can increase anxiety about sleep.
- Cognitive Behavioral Therapy for Insomnia (CBT-I): This structured therapeutic approach is highly effective for treating insomnia. It helps you identify and challenge negative thought patterns about sleep, develop healthy sleep habits, and establish a positive sleep routine.
- Consider Professional Help: If your insomnia persists despite your efforts, consult a healthcare provider. They might recommend behavioral therapies, prescribe medications for a short duration, or investigate underlying medical or psychological factors.
- Keep a Sleep Diary: Track your sleep patterns, daily routines, and any factors that might affect your sleep. This can help you and your healthcare provider identify patterns and potential triggers.
Remember that overcoming insomnia is a gradual process, and what works for one person might not work for another. Be patient with yourself and give your body time to adjust to new habits. If your insomnia is severely affecting your quality of life, don’t hesitate to seek guidance from a healthcare professional who can provide personalized recommendations and support.
Sore Throat, Symptoms, Causes, Prevention & Home Remedies
Dandruff: Types, Symptoms, Causes & Prevention
Dark Circles Under Eyes: Symptoms, Remedies & Prevention
Heart Attack: Types, Symptoms & Prevention
Eye Infections: Symptoms, Causes & Treatment
Vertigo: Causes, Symptoms, Treatment & Preventive
Hair Loss, Types, Symptoms, Prevention & Treatments
Knee Pain, Symptoms, Types & Self Management
Read this Article Also:- Yoga Nidra for Sleep
If you don’t like this article/post please share your feedback.